Warmer weather is a time when flowers are blooming, pollen is in abundance and grasses are at seed. In other words, an absolute nightmare if you experience allergies, hay fever or histamine intolerance/sensitivity.
But did you know that this season of horror could be associated with the health of your gut? Yes, that’s right. Your sneezing, red eyes and runny nose could be alleviated by changing your gut health.
How does histamine affect the body?
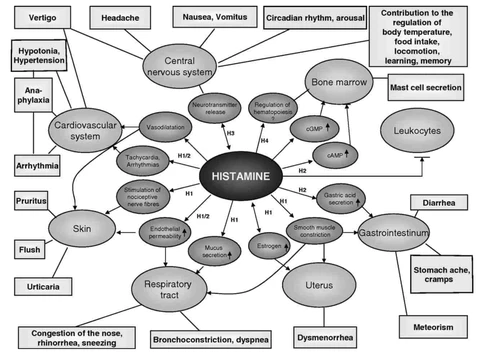
Histamine exerts its effects by binding to its four receptors. Histamine 1 receptor (H1R), H2R, H3R, and and H4R, which are located on target cells in various tissues (1).
Your gut role in breaking down histamine
One way your gut is connected to your nose is through an enzyme called diamine oxidase (DAO). DAO enzymes are made and stored along your small and large intestine.
When you eat histamine containing or producing foods DAO assists in it’s breakdown which reduces the amount absorbed into your bloodstream. When there is a reduction in DAO it may cause an increase in histamine absorption, resulting in histamine accumulation (1).
Gut-Histamine Connection
So what impacting this enzyme? Many gut condition are associated with high amounts of inflammation in the gut wall. This inflammation causes damage to the cells that produce and store DAO (1)
-
Inflammatory Bowel Disease (Crohn’s Disease and Ulcerative Colitis) have been shown to have increased levels of histamine as well as increased mast cell (immune cells that can release histamine) numbers in their gut (2)
2. Small Intestinal Bacterial Overgrowth (SIBO) cause inflammation in the gut due to an increase in toxin release (specifically one called lipopolysaccharide), inflammatory cytokine production (proteins that work in immune signalling) and immune activation (3). The presence of these can also lead to mast cell degranulation (leak/release), which leads to excessive production of histamine (4,5).
3. Irritable Bowel Syndrome (IBS) patients have a strong association with SIBO (approximately 80% overlap) (6) and tend to have higher amounts of histamine levels, which are correlated with their abdominal pain (2 7). People with IBS also tend to report a worsening of their symptoms from histamine-rich and histamine-releasing foods.(8)
4. Alcohol, non-steroidal anti-inflammatory drugs and antibiotics have also been shown to suppress DAO production and all have the potential to cause inflammation to the gut mucosa (hello leaky gut) (1).
5. Dysbiosis (imbalance) of gut bugs have the potential to convert histidine to histamine in food leading to excess production, e.g. Streptococcus thermophiles, Lactobacillus delbrueckii, Lactobacillus bulgaricus, Lactobacillus reuteri, Lactobacillus brevis and Lactococcus lactis. An overgrowth of these or excessive consumption of these (fermented foods or probiotics) may exacerbate symptoms. An overgrowth of E. coli many also lead to increased production of histamine (9).
How to treat a histamine intolerance/sensitivity
It’s complicated and usually needs qualified assistance, but some tips to get you started are:
-
Check your medications. Many over-the-counter and prescribed medications that affect DAO either directly or indirectly, drugs that decrease DAO activity should be avoided (e.g. NSAIDS and antibiotics) (1). This must be done with the consultation and guidance of a qualified practitioner.
-
Support nutrients that help DAO enzyme production, such as zinc, vitamin C and vitamin B6.
-
Whilst finding help in addressing the root cause, remove foods that are known to exacerbate symptoms.
-
Be wary of the probiotics you supplement with, opt for strains other than histamine producers mentioned above, including bifidobacteria species found in COYO products!
-
Join Rachel’s course Bloated to Body Confident to help you address the root cause of your histamine issues (SIBO, dysbiosis, leaky gut etc). Visit her website here.